Introduction
Infection control is a critical aspect of any healthcare setting, particularly in dental clinics where the risk of cross-contamination is high. Modern clinics must adhere to stringent infection control protocols to ensure the safety of patients and staff.
Definition
The procedures and guidelines put in place to stop infections from spreading in dental settings are referred to as dental infection control. Using personal protective equipment (PPE), sterilising tools, and strict cleanliness protocols are all part of it to reduce the possibility of pathogen transmission between patients and dental healthcare professionals. Efficient management of infections guarantees a secure setting for dental operations and shields patients and dental personnel from any infections.
Understanding the Importance of Infection Control
“Infection control in dental clinics is vital to prevent the spread of infectious diseases” says Enhanced Dental Studios. Dental procedures often involve exposure to blood, saliva, and other bodily fluids, making both patients and healthcare workers susceptible to infections if proper precautions are not taken. Effective infection control not only protects the health and well-being of everyone in the clinic but also upholds the clinic’s reputation and legal compliance.
Hand Hygiene: The First Line of Defense
The most fundamental but important infection prevention technique is good hand hygiene. The Centers for Disease Control and Prevention (CDC) emphasizes the importance of regular handwashing with soap and water or using an alcohol-based hand sanitizer. In a dental clinic, staff should wash their hands:
-
Before and after treating each patient
-
Prior to putting on gloves and right away after taking them off
-
After coming into contact with any possibly contaminated surface or object
Encouraging patients to sanitize their hands upon entering the clinic also adds an extra layer of protection.
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) is essential for preventing the transmission of infectious agents during dental procedures. The standard PPE in dental settings includes gloves, masks, protective eyewear, and gowns.
-
Gloves: Always wear gloves when performing dental procedures or handling instruments. Gloves should be changed between patients and discarded immediately after use.
-
Masks: Surgical masks stop drips from spreading and shield the wearer from airborne contaminants. Masks should be worn at all times during patient treatment and changed regularly.
-
Protective Eyewear: Safety glasses or face shields protect against splashes of blood or saliva. They should be cleaned and disinfected after each use.
-
Gowns: Wearing disposable or reusable gowns helps protect clothing and skin from contamination. Gowns should be changed if they become visibly soiled.
Instrument Sterilization and Disinfection
Sterilization and disinfection of dental instruments are non-negotiable aspects of infection control. It is imperative to properly clean and sterilise any instruments that come into touch with blood or mucous membranes prior to their reuse.
-
Cleaning: Instruments should first be cleaned with an enzymatic cleaner to remove organic material. Ultrasonic cleaners are often used to enhance this process.
-
Sterilization: Autoclaves are the gold standard for sterilizing dental instruments. They use steam under pressure to kill all forms of microbial life, including spores. Instruments should be packaged before sterilization to maintain sterility until they are used.
-
Disinfection: Non-critical items, such as dental chairs and countertops, should be disinfected between patients using EPA-registered disinfectants that are effective against a broad spectrum of pathogens.
Environmental Cleaning and Disinfection
In addition to instrument sterilization, environmental cleaning plays a significant role in preventing infections. Surfaces in the dental clinic, particularly those that are frequently touched, must be regularly disinfected.
-
Treatment Rooms: Dental chairs, light handles, and other surfaces in the treatment area should be disinfected after each patient. Barrier protection (e.g., plastic covers) can be used on equipment that is difficult to clean.
-
Common Areas: Waiting rooms, restrooms, and reception areas should be cleaned multiple times a day. High-touch surfaces like doorknobs, countertops, and pens should receive special attention.
-
Ventilation: Proper ventilation reduces the concentration of airborne contaminants. Clinics should ensure that their HVAC systems are well-maintained and consider using HEPA filters and UV light systems to enhance air quality.
Safe Handling and Disposal of Waste
Proper management of dental waste is crucial to infection control. This covers the getting rid of hazardous materials, biological waste, and sharps.
-
Sharps Disposal: Needles, scalpels, and other sharp instruments should be disposed of in puncture-resistant sharps containers immediately after use. These containers should be clearly labeled and located as close as possible to the area of use.
-
Biological Waste: Materials contaminated with blood or bodily fluids should be disposed of in biohazard bags. These bags should be sealed and stored in a designated area until they can be safely removed by a medical waste disposal service.
-
General Waste: Regular clinic waste should be disposed of daily, with care taken to avoid overfilling trash bins. After handling any garbage, one should wash their hands.
Patient Safety and Education
Educating patients about infection control practices is essential. Patients should be informed about the measures the clinic is taking to ensure their safety, such as the use of PPE and sterilization protocols. Additionally, patients should be encouraged to report any symptoms of infectious diseases before their appointments, allowing the clinic to take appropriate precautions.
Staff Training and Compliance Monitoring
Ongoing staff training is vital to maintain high standards of infection control. Dental staff should be regularly updated on the latest guidelines and protocols. Training should cover hand hygiene, PPE use, instrument sterilization, and waste disposal.
Compliance monitoring ensures that infection control practices are consistently followed. This can include regular audits of sterilization procedures, observation of hand hygiene practices, and checking that PPE is worn correctly. Any lapses should be addressed immediately with additional training or corrective actions.
Managing Respiratory Infections
Given the nature of dental procedures, managing respiratory infections is particularly important. Dental clinics should screen patients for symptoms of respiratory infections and consider rescheduling appointments for those who are ill. In some cases, treatment can proceed with enhanced precautions, such as the use of high-filtration masks and air purifiers.
Adapting to Emerging Infectious Threats
The COVID-19 pandemic highlighted the need for dental clinics to be adaptable in their infection control practices. Clinics should have protocols in place for responding to emerging infectious threats, which may include heightened screening procedures, the use of additional PPE, and modifications to clinic layouts to allow for social distancing.
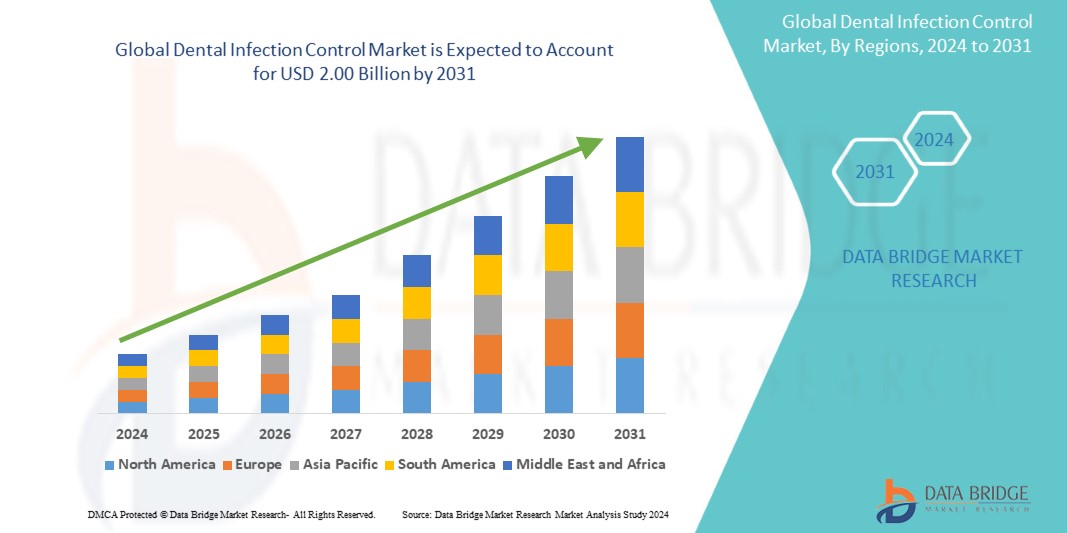
Growth Rate of Dental Infection Control Market
The size of the worldwide market for dental infection control was estimated at USD 1.30 billion in 2023 and is expected to grow at a compound annual growth rate (CAGR) of 5.5% from 2024 to 2031, reaching USD 2.00 billion.
Read More: https://www.databridgemarketresearch.com/reports/global-dental-infection-control-market
Conclusion
Dental infection control is a dynamic and essential component of modern clinical practice. By adhering to these best practices, dental clinics can protect both their patients and staff from infectious diseases, ensuring a safe and professional environment for dental care. Regular review and adaptation of infection control protocols are crucial to staying ahead of potential threats and maintaining the highest standards of patient safety.